
Osteochondrosis is one of the most common diseases of the spine. It is believed that it mainly occurs in the neck or waist. After all, it is in these places where the spine is very flexible and under great pressure. But most people's sedentary lifestyle and long time sitting at the dining table have caused thoracic spine osteochondrosis to occur more and more frequently. Although in many cases, this pathology will not be diagnosed immediately. After all, the characteristic of thoracic osteochondrosis is that its symptoms are non-specific and similar to many other pathologies.
General characteristics
This degenerative dystrophy affects the intervertebral discs of the thoracic spine. This is due to a violation of the metabolic process, resulting in the thinning and drying of cartilage tissue. As a result, under the influence of physical exertion, the disc began to collapse and lose its devaluation function. The vertebrae, ligaments and joints in the spine are gradually affected. Nerve fibers and blood vessels may be damaged.
This process develops slowly, so pathology is difficult to diagnose. Moreover, not everyone sees a doctor immediately, because they don't know the hazards of thoracic osteochondrosis. But if left untreated, this disease can lead to serious complications. Since this part of the spine is responsible for the blood supply and innervation of internal organs, various pathologies can develop with the advanced form of thoracic osteochondrosis. Intestinal peristalsis, the work of the heart, liver and digestive tract are disturbed. Pancreatitis, cholecystitis, and biliary dyskinesia may occur. But the most common complication occurs in the spine. In addition to herniated disc and intercostal neuralgia, there can also be spinal cord compression, spondylopathy, sciatica, and postural disorders.
Thoracic osteochondrosis is also common in men and women. Its appearance does not even depend on age, although degenerative malnutrition was previously thought to be characteristic of the elderly. However, due to improper diet and sedentary lifestyle, modern young people are increasingly suffering from osteochondrosis.
It is believed that the most common osteochondrosis is cervical spondylosis. Usually, pathology also occurs in the waist area. This is due to the special structure of the bones. In the thoracic region, the spine has lower mobility because it is connected to the ribs and sternum.
The discs here are thinner and the vertebrae are closer together. But this part is less susceptible to injuries and other external influences, because part of the load is borne by the ribs and chest.
Osteochondrosis usually occurs at the level of the 7-11 vertebrae. In this case, the intervertebral disc is mainly affected. In most cases, 1-2 segments of the spine will be affected. But sometimes multi-segment osteochondrosis occurs, in which multiple intervertebral discs are destroyed at the same time. Rarely, this part of the pathology occurs independently, usually combined with cervical or lumbar disease. In this case, the symptoms are more pronounced, so it is easier to diagnose the disease.
The characteristic of thoracic osteochondrosis is that it rarely manifests as back pain after exertion, which is the case when it is located in the cervical or lumbar spine. The initial pathology is confused with heart or lung disease. After all, the pain is often confined to the chest, shortness of breath, nausea, and chills. However, the manifestations of thoracic osteochondrosis are not very obvious, so patients do not always see a doctor in the initial stage. Therefore, the pathology progresses.
Disease development
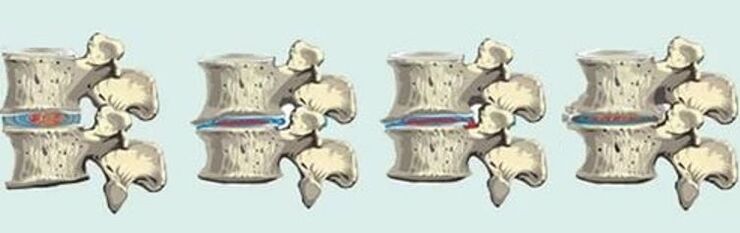
The danger of thoracic osteochondrosis is that it is "disguised" as another disease. The pathology develops slowly, and few patients seek medical attention at the initial stage. Osteochondrosis begins with thinning of the intervertebral discs. Its core flattened, its outer shell cracked and dried out, and its vertebrae moved closer together. There is usually no major discomfort at this stage, only slight muscle tension. If the disease can be detected, it can be completely cured by restoring the condition of the intervertebral disc.
But usually the progression of osteochondrosis will continue. In the surrounding soft tissues, the inflammatory process may begin and the joint capsule is damaged. The mobility of the spine is reduced and the vertebrae may be displaced. If you continue to increase physical activity, because the vertebrae rub against each other, they will appear microcracks. At this time, there is a squeezing sensation in the chest, and the upper body hurts as soon as he moves.
In the third stage of osteochondrosis, the intervertebral disc becomes very thin, with protrusions and hernias. The mobility of the spine is almost completely restricted. Osteophytes begin to form on the vertebrae. This stage is characterized by obvious nerve root syndrome, because nerve fibers are damaged. In this case, the work of the internal organs is severely disturbed. In most cases, it is at this time that the patient sees the doctor and begins treatment. If you don't do this, complications can lead to disability, and when the spinal cord is compressed, you can't move at all.
The final stage of osteochondrosis is characterized by complete destruction of the intervertebral disc and loss of function. The bone tissue of the vertebrae begins to collapse, so the mobility of the spine is completely impaired. All the vegetative and nerve root symptoms of thoracic osteochondrosis are obvious.

The development of thoracic osteochondrosis is fluctuating. This is usually a slow, chronic process with little discomfort. May increase fatigue and weakness. When exposed to external factors, severe pain worsens. In this case, the patient usually needs to be hospitalized because the attack may be accompanied by lack of air, difficulty breathing, chest pain, or abdominal pain.
reason
Like other forms, the main cause of thoracic osteochondrosis is a disorder of mineral metabolism. Due to the process of degenerative dystrophy, herniated or herniated discs appear, they become thinner and stop performing their functions, the vertebrae gradually collapse and osteophytes grow. This is usually due to an unbalanced diet, leading to a lack of essential nutrients, or age-related changes in the composition of cartilage tissue. Degeneration of the intervertebral disc can also lead to poor spinal circulation, bad habits, or genetic predispositions.
But lack of minerals does not always cause osteochondrosis. This requires predisposing factors that affect the spine itself.
Therefore, the following causes of this pathology are also different:
- The spine is often subjected to static loads;
- Sitting in an uncomfortable position on the table for a long time;
- weightlifting;
- obesity;
- Injury to the spine or surrounding tissues;
- Engage in power sports;
- Prickly pear;
- Muscle corset weakness;
- Congenital bone deformities;
- Severe hypothermia;
- Excessive tension.

Facts have proved that people who are in uncomfortable positions for a long time at the dining table or while driving, as well as those engaged in manual labor, are most prone to pathological changes. In fact, the increased load and no load at all are equally harmful to the intervertebral disc.
In addition, osteochondrosis usually occurs in young people with osteochondrosis. This pathology usually occurs in the lower chest area of adolescents. It is characterized by vertebral spongy tissue necrosis, spinal deformity, and neurological symptoms. As the pathology progresses, it will be complicated by osteochondrosis.
Pathological manifestations
The main symptoms of thoracic osteochondrosis are pain, nerve root syndrome and visceral dysfunction. This pathological pain may be severe, paroxysmal or painful, continuous, and increase with exercise. Sometimes patients are admitted to hospital for suspected acute pancreatitis, cholecystitis, or urinary tract stones. After all, pain is not always confined to the affected vertebral area. Therefore, thoracic osteochondrosis is often mistaken for other organs.
In addition, the degenerative process of the spine in this disease is almost always accompanied by vascular disease or intercostal neuralgia. This is due to the special structure of the spine in this section-the distance between the vertebrae is very small, and there are a lot of nerves and blood vessels.

By limiting the mobility of the upper body and increasing bending, sternal osteochondrosis can be suspected. Intercostal neuralgia often occurs. Acute pain can last for several hours or more. It can be triggered by lifting weights, maintaining a static posture for a long time, and hypothermia.
If the blood vessels are affected, it will destroy the blood supply and nutrients to the skin. As a result, the fragility of the nails increases, and the skin becomes dry and peeling. Cold skin and cold limbs are often observed.
Characteristics of pain
The pain of thoracic osteochondrosis may vary in intensity and location. Pain usually occurs between the chest or shoulder blades. They can be aggravated by raising their arms, turning or bending their bodies, coughing or sneezing. The pain can be severe, urgent, or painful.
Usually, this feeling is divided into two groups: back pain and back pain. Dorsago is an episode of acute pain between the shoulder blades. Also known as "chest and back pain". The pain is so severe that the patient cannot move. Dorsal attacks usually occur after a long period of rest during the first exercise. Accompanied by muscle cramps, respiratory function is impaired. The sensation extends to the shoulder blades and between the ribs to the chest. Chest pain caused by osteochondrosis is similar to an angina pectoris, but unlike this, nitroglycerin cannot eliminate it. In addition, the pain increases when pressing the vertebrae.
Back pain is chronic mild pain. It usually starts gradually and there is slight discomfort in the thoracic spine. In this case, the pain will increase when bending, turning, raising the arm or even walking. This severely limits the patient's mobility. In addition, after deep breathing, sitting for a long time, or at night, the pain can be observed to increase. Back pain can last from 2 weeks to a month. Chest tightness and shortness of breath may resemble pneumonia, but the patient does not have a cough or fever.

Nerve root syndrome
When the vertebrae or spastic muscles of the nerve root are compressed, the signs of osteochondrosis in the thoracic spine area become more obvious. After all, the spinal nerves located in this part of the spine are responsible for the innervation of the skin, the motor functions of the limbs, and the functions of the internal organs.
In addition to tingling in the back, chest, or abdomen, nerve compression is accompanied by the following symptoms:
- Paralysis or partial paralysis of limbs;
- Violation of skin sensitivity;
- Numbness, burning, tingling, "goose bumps" feeling when running;
- Violation of the tendon reflex;
- Reflex muscle spasms;
- Nutritional changes of the skin-hair loss, discoloration, dryness and flaking.
The intensity of these symptoms increases with physical exertion, deep breathing, sedentary sitting, hypothermia, or stress.

Plant barriers
There are a large number of nerves and blood vessels in the thoracic spine, which ensure the normal function of internal organs. Therefore, for osteochondrosis, various autonomic disorders must be observed. They depend on the location of the affected vertebrae and the pathological stage.
Spine lesions in the upper thoracic area, discomfort in the esophagus, and coma in the pharynx. Difficulty swallowing, voice changes may occur. The middle thoracic spine is responsible for the liver, gallbladder, stomach and pancreas. Therefore, when they are destroyed, symptoms similar to pancreatitis, cholecystitis or gastritis often appear. If the degenerative changes affect the lower thoracic spine, there may be problems with the intestines and genitals.
Patients often see a doctor for abdominal pain. They usually get worse at night or after manual labor. In addition, pain has nothing to do with the patient's dietary characteristics. This gastric syndrome is characteristic of sternal osteochondrosis. However, despite abdominal pain, ruptured intestines, nausea and flatulence, no problems with the work of the digestive tract were found. These feelings stem from damage to the spinal nerves and blood vessels.
diagnosis
Because the symptoms of thoracic osteochondrosis are non-specific, the pathology can only be found through a comprehensive examination. At the same time, it is also important to distinguish it from other diseases. X-ray or tomography of the spine can help rule out spondylosis, rheumatoid arthritis, and ankylosing spondylitis.
But other inspection methods are needed. This is a urine test, whole body blood test and biochemical test, fluoroscopy, electrocardiogram, MRI or visceral ultrasound. This test can rule out pancreatitis, gastritis, gastric ulcer, heart disease, pneumonia, and urolithiasis.

treatment
The treatment of thoracic osteochondrosis should be comprehensive. Since the pathological cause is a degenerative process, it is impossible to completely cure it. Only in the initial stage, when the vertebral structure has not been disturbed, and the intervertebral disc is only slightly reduced, can this process be stopped and the function of the spine can be restored.
However, the treatment of thoracic osteochondrosis is usually aimed at slowing down tissue destruction, relieving pain and neurological symptoms, and restoring mobility. The choice of treatment depends on the pathological stage, the location of the degenerative process, and the symptoms exhibited. It is necessary to start treatment as soon as possible so that there are more opportunities to avoid complications.
It is especially important to see a doctor when the back pain is severe and the ejaculatory pain radiates to the chest or scapula. This deterioration can be eliminated by special methods. These drugs are usually used in the form of tablets or injections, various ointments or dressings, and physical therapy procedures. The spine must also be fixed: show the patient several days of bed rest and limited mobility.
After the seizure is resolved, treatment will not stop. But now its main goal is to stop the degradation process and restore tissue nutrition. Among the drugs used for this, chordal protectors, vitamins and means to improve metabolism are used. In addition, courses of massage and physiotherapy procedures and physiotherapy exercises must be prescribed. Moreover, the implementation of special drills must be continuous. In order to prevent complications, it is necessary to monitor the diet in order to provide the body with all the necessary vitamins and minerals. Lifestyle is also important: choosing the right mattress and pillows for sleeping, working chairs, alternating rest and physical activity.
Thoracic osteochondrosis is a very serious pathology, and if left untreated, it can lead to dangerous complications. However, the difficulty of diagnosis causes the disease to progress frequently. Therefore, it is very important to develop a correct lifestyle and avoid the factors that lead to the damage of the intervertebral disc. This will help prevent the development of osteochondrosis and keep the spine healthy.

























